News and Announcements
Stay connected, stay ahead. Know everything that matters, as it happens. From the very latest industry news, reports, papers, and studies. Would you like to see your news here? Email the admin and we will get it linked.

Scientific Workshops are interactive discussions covering the latest scientific developments in a range of hematologic topics. The 2025 Scientific Workshops will take place on Friday, December 5, and will also be streamed on the ASH annual meeting platform for virtual participants.
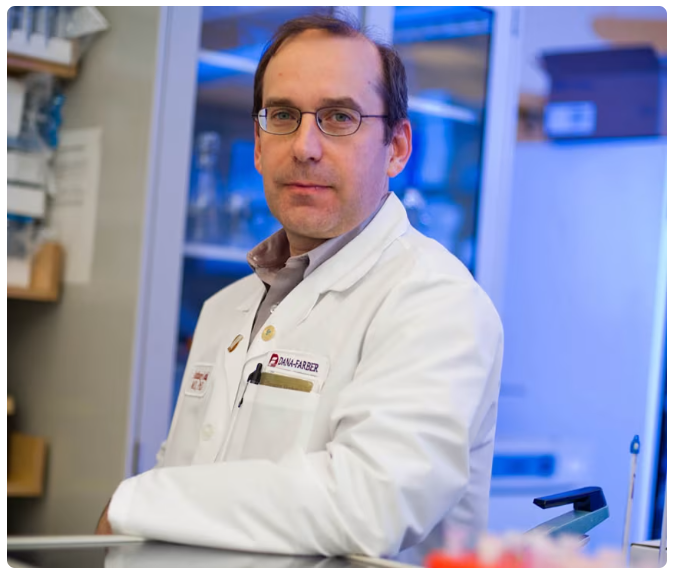
Anthony Letai, MD, Ph.D., was sworn in today as director of the National Cancer Institute (NCI), part of the National Institutes of Health (NIH), by Health and Human Services Secretary Robert F. Kennedy, Jr.
Dr. Letai takes the helm of the world’s most prestigious cancer research agency after serving as professor of medicine at Harvard Medical School and medical oncologist at the Dana-Farber Cancer Institute. He possesses decades of experience studying cell death in cancer, developing treatments, and identifying predictive biomarkers.

In this riveting talk, SFPM Board Member Dr. Diana Azzam, a cancer researcher and the Scientific Director of the Center for Advancing Personalized Cancer Treatments at Florida International University, shows how functional precision medicine and AI can be used to develop individualized treatmentplans for patients who have exhausted standard cancer care. By testing each patient’sown cancer cells to find treatments that work best for them, her work bridges research and clinical care, bringing hope to cancer patients through personalized medicine. Diana Azzam, PhD is a cancer researcher and Scientific Director of the Center for Advancing Personalized Cancer Treatments at Florida International University. Her lab uses functional precision medicine and AI to develop individualized treatment plans for patients who have exhausted standard care--testing each patient’s own cancer cells to find treatments that work best for them. Her work bridges research and clinical care, bringing hope to cancer patients through personalized medicine. This talk was given at a TEDx event using the TED conference format but independently organized by a local community.
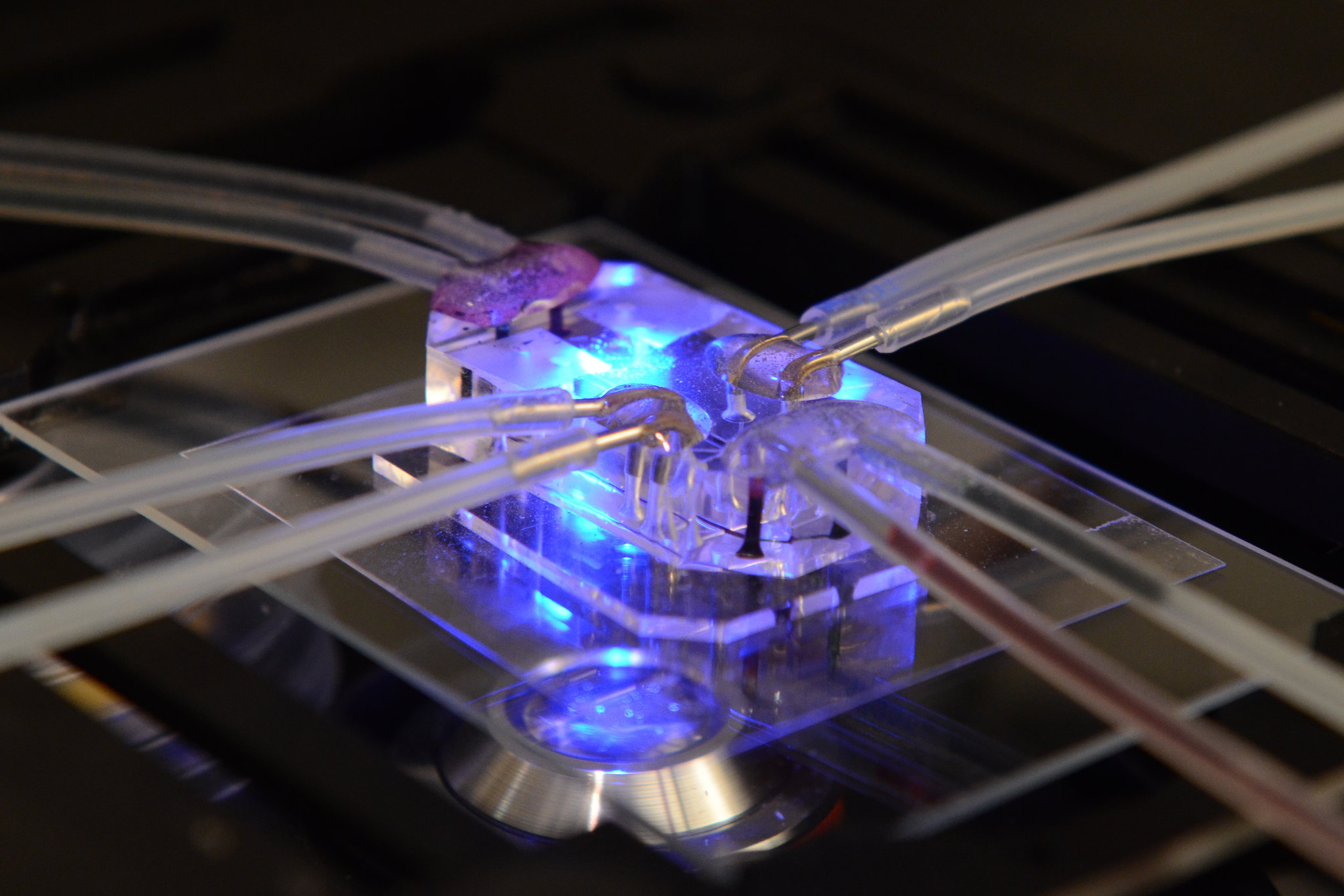
In recent announcements, the United States National Institutes of Health announced that it wants to prioritize human-based research technologies. In a key adjunct to this initiative, it stated that it would no longer develop funding opportunities focused solely on animal models of human disease. The NIH release specifically mentions the use of “organoids, tissue chips and other in vitro systems that allow scientists to model human disease and capture human variability and patient-specific characteristics.” Members of the Society for Functional Precision Medicine should recognize that this announcement will likely increase the interest in their work, as nearly all members are developing human based models. The SfPM suggest that members stay alert for NIH funding opportunities that may later accompany this new initiative, as well as for signs that other countries are moving in the same direction. Australia is an example of a country whose national science agency (CSIRO) has previously reported favorably on the use of non-animal models.
The terms “non-animal models” and “human models” are starting to be used interchangeably. Examples of human models in which members of the Society of Functional Precision Medicine have expertise include organoids, 2D cultures, spheroids, organ on chip or tumor on chip, implantable microdevices, single cell suspensions, and tissue slices.

Cell density, the ratio of cell mass to volume, is an indicator of molecular crowding and a fundamental determinant of cell state and function. However, existing density measurements lack the precision or throughput to quantify subtle differences in cell states, particularly in primary samples. Here we present an approach for measuring the density of 30,000 single cells per hour by integrating fluorescence exclusion microscopy with a suspended microchannel resonator.

Eighty-five percent of diagnosed cases of lung cancer are non-small cell lung cancer (NSCLC). In this group, 5% of patients show molecular alterations in the ALK gene involved in cell multiplication. The use of inhibitors against this oncogene — one of the most effective strategies against this type of cancer — has benefited many patients. But, is it possible to know if the treatment will be effective in all those affected?

The B-cell lymphoma 2 inhibitor venetoclax has shown promise for treating acute myeloid leukemia (AML). However, identifying patients likely to respond remains a challenge, especially for those with relapsed/refractory (R/R) disease. We evaluated the utility of ex vivo venetoclax sensitivity testing to predict treatment responses to venetoclax-azacitidine in a prospective, multicenter, phase 2 trial.
Key Points:

This year during two days in October, the 3rdPrecision Medicine Networking forum took place in Riga, Latvia. For the second time this forum included a special session for Functional precision medicine, organized by SfPM member Inese Cakstina-Dzerve, RSU, Latvia (former Fulbright fellow at Letai lab). This session was co-chaired with speaker from last year -Caroline Heckman (FIMM, Helsinki, Finland). A speaker team consisted of 2 SfPM board members (Diana Azzam and Christian Regenbrecht) and 2 Letai lab alumni(Triona Ni Chonghaile and Inese Cakstina-Dzerve).

The Society recently held elections for several open seats including two newly created seats which aim to include commercial sector representation.
Congratulations to our newest board members:
The following members have been reelected for another term:
Click the button below to learn more about our board.

Many SFPM stalwarts will be speaking at the PMNET meeting October 10-11, Riga Latvia. Please visit pmnetforum.com to register for this exciting meeting!